Vulvodynia Treatments
Vulvodynia is not simply a gynecological disorder and experts typically recommend a multidisciplinary approach. It is a chronic pain condition of the vulva, and if you don’t experience adequate relief with treatment prescribed by your gynecologist, treatment by a women’s health physical therapist and/or a pain management specialist can be very helpful. Since chronic pain can lead to depression, you may benefit from sessions with a therapist, specifically one who can teach cognitive behavior therapy. A recent review of the research recommended both physical therapy and cognitive behavior therapy for women suffering from vulvodynia.
Researchers have made substantial progress toward understanding the causes of vulvodynia. We are hopeful that pharmaceutical companies will develop vulvodynia-specific treatments within the next decade.
At this time, there is no single treatment that helps every woman with vulvodynia. Finding the best treatment, or combination of treatments for you is a trial and error process. While you are trying a new treatment, it is helpful to keep a pain journal to evaluate its effectiveness. (Please remember that oral medications can take 3 to 4 weeks to start working.)
A general resource guide on chronic pain medications and treatments has been developed by the American Chronic Pain Association and Stanford Medicine. Advice specific to vulvodynia follows.
- Discontinuation of Irritants: Health care professionals recommend eliminating over-the-counter feminine products such as perfumed bubble baths, soaps, sprays and douches that can irritate vulvar tissue. Eliminating irritants is typically the first step in treatment. (Please see Self-Help Strategies for additional information.)
- Oral “Pain-Blocking” Medications: Medications that are effective in alleviating other chronic pain conditions are often used in the treatment of vulvodynia. They include:
- Tricyclic Antidepressants (TCAs): Even though TCAs were developed to treat depression, they have also been used to treat chronic pain. Until the 2000s, TCAs were one of the most common treatments for vulvodynia because of their widespread use in treating other chronic pain conditions. Then a large NIH-funded study found that the TCA desipramine was no more effective than a placebo for relieving vulvodynia. They are not widely used today, because of this study and the fact that TCAs have more undesirable side effects than newer pain-relieving medications.
If your doctor prescribes a TCA, you should be aware of the following. TCA dosage for chronic pain, including vulvodynia, is much lower than the dosage used for depression. To minimize side effects, it is best to start at a very low dose and increase the amount gradually; consequently, it can take several weeks to achieve a therapeutic level. Common side effects, which can usually be managed, include drowsiness, dry mouth, constipation and dizziness. The severity of the side effects depends on which TCA you take, e.g., amitriptyline causes stronger side effects than nortriptyline or desipramine. If you decide to stop taking a TCA, it should be discontinued gradually.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): SNRIs, a relatively new type of antidepressant, work differently than the TCAs. These medications are FDA-approved to treat depression and anxiety disorders, as well as certain types of pain, such as fibromyalgia and peripheral neuropathy. SNRIs are also used “off-label” to treat other chronic pain disorders. The most common side effects, some of which improve over time, include headache, nausea, insomnia, sexual dysfunction, dry mouth and dizziness. It can take 4 to 6 weeks for this medication to take effect. If you decide to discontinue a SNRI, you have to taper it slowly. Two SNRIs, venlafaxine and duloxetine, have been used to treat vulvodynia, but their effectiveness has not been tested in large controlled studies.
- Anticonvulsants: Medications developed to inhibit seizures can also be effective in controlling some chronic pain syndromes. For example, the anticonvulsant pregabalin is FDA-approved to treat post-herpetic neuralgia and diabetic neuropathy. Anticonvulsants are often prescribed for women with vulvodynia, especially when pain is described as having a “shooting, stabbing or knife-like” component. The only controlled study on the effectiveness of anticonvulsants for vulvodynia found that gabapentin (Neurontin) was no more effective than a placebo. However, many doctors continue to prescribe it. As with TCAs, it is best to start at a very low dose and increase the amount gradually. If you decide to discontinue an anticonvulsant, you have to taper it slowly.
- Opioids: Pain-relieving opioids, such as oxycodone and hydrocodone, can be helpful for short-term use during vulvodynia flares. They can also be used to relieve pain early in treatment, while you gradually increase the dosage of an antidepressant or anticonvulsant to a therapeutic level. In severe cases, when more conservative therapies fail to provide relief, long acting opioids can be used. Common side effects, which can usually be managed, include constipation, nausea and drowsiness. If you take an opioid occasionally for short-term flares, it is unlikely to cause addiction. Relying on an opioid for long-term pain relief does cause addiction, so it must not be discontinued abruptly.
- Tricyclic Antidepressants (TCAs): Even though TCAs were developed to treat depression, they have also been used to treat chronic pain. Until the 2000s, TCAs were one of the most common treatments for vulvodynia because of their widespread use in treating other chronic pain conditions. Then a large NIH-funded study found that the TCA desipramine was no more effective than a placebo for relieving vulvodynia. They are not widely used today, because of this study and the fact that TCAs have more undesirable side effects than newer pain-relieving medications.
- Topical Medications: Topical medications applied directly to the vulva can help to alleviate pain, but some preparations contain additive substances that are irritating to the skin. Therefore, many vulvodynia experts use compounding pharmacies that make individualized topical creams and ointments without irritating additives. Examples include:
- Topical Hormonal Creams (e.g., estrogen, testosterone): Topical estrogen cream can improve the health of vulvar tissue, particularly when the tissue is thin or dry because of a lack of estrogen. Recently, some experts have also emphasized the role of the hormone testosterone for women’s sexual health and recommend combining estrogen and testosterone in a topical cream.
- Topical Anesthetics (e.g., lidocaine): Topical anesthetic cream or ointment provides temporary pain relief and is applied directly to the vulva prior to intercourse. Typically, the numbing effect lasts 15 to 30 minutes. One study found that long-term nightly use of lidocaine resulted in sustained pain relief.
- Topical Compounded Formulations: Medications that are normally prescribed for oral use, such as antidepressants and anticonvulsants, can also be formulated into a cream or ointment. Topical preparations either contain a single active ingredient or a combination of ingredients, e.g., an anesthetic and antidepressant. Compounded topical formulations may be used in conjunction with oral medications and other treatments.
- Pelvic Floor Muscle Therapy

Courtesy of Dr. Howard GlazerSome women with vulvodynia also have pelvic floor muscle weakness or spasm. In addition to evaluating pelvic floor muscles, a physical therapist should assess joints, muscles and nerves in the lower half of the body to determine if they play a role in vulvar pain. Treatments include exercise, education, and manual therapies, such as massage, soft-tissue work and joint mobilization. Modalities such as heat/cold, ultrasound and electrical stimulation may also be helpful.
In addition, rehabilitation of the pelvic floor muscles may include insertion of a vaginal sensor and the use of a biofeedback machine (pictured on right). The machine provides visual feedback on the strength of pelvic floor muscles while performing exercises to normalize their function. This type of biofeedback is conducted by specially trained providers and some physical therapists. You can access NVA ‘s referral list (www.nva.org) to find physical therapists who specialize in treating vulvodynia and pelvic floor muscle dysfunction.
- Nerve Blocks
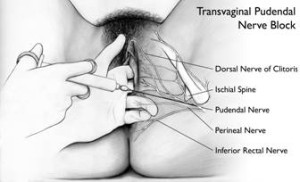
Courtesy of Dawn Danby and Paul WaggonerThe pudendal nerve, located in the pelvis, carries sensations from the vulva to the brain. A pudendal nerve block injection uses local anesthetic and a steroid to numb the nerve and interrupt the transmission of pain signals. In many cases, a series of injections, spaced days or weeks apart, is administered intravaginally (pictured to the right) or in the epidural space in the lower back (same technique used during childbirth). Many women experience short-term relief with this procedure and some experience long-term relief. One recent study found that women with vulvodynia who underwent a series of different nerve blocks (vulvar, pudendal and spinal) experienced sustained pain relief.
- Diet Modification: Some women find that eating a certain food increases their pain and that elimination of the food alleviates it. For example, some eliminate acidic or high-sugar foods. If you want to test for food sensitivity, eliminate one item or food group at a time, so you can determine which ones, if any, are affecting you. With the use of a food diary, you may begin to notice an association that you wouldn’t otherwise suspect.
- Neurostimulation and Spinal Infusion Pump: In severe cases, when more conservative forms of treatment haven’t worked, neurostimulation or implantation of a spinal infusion pump may be recommended. Neurostimulation involves the implantation of an electronic device that delivers low voltage electrical stimulation to the spinal cord, or a targeted peripheral nerve, with the intent of substituting a tingling sensation for pain. Spinal infusion pumps continually administer very small amounts of medication to the spinal cord and nerve roots. For additional information on these treatment methods, please visit: https://www.columbianeurosurgery.org/treatments/neuromodulation/.
- Counseling: Since living with chronic vulvar pain usually affects a woman’s sexual relationship and can lead to anxiety and/or depression, some women find it helps to see a psychologist or a couples/sex therapist.
- Complementary or Alternative Medicine: Women with vulvodynia, as with all forms of chronic pain, may benefit from using alternative therapies in conjunction with traditional medical treatments. There are many complementary therapies available, such as acupuncture, massage therapy, relaxation techniques and cognitive behavior therapy. To learn about complementary treatments, please visit the National Center for Complementary and Alternative Medicine’s web site.
- Surgery for women with Provoked Vestibulodynia (formerly known as Vulvar Vestibulitis Syndrome): Surgery is contraindicated for women with Generalized Vulvodynia. Two surgical procedures are used for women with PVD. Vestibulectomy with vaginal advancement involves the removal of a portion (or all) of the vestibule, including the hymen, followed by vaginal advancement. In a modified vestibulectomy, only the superficial painful tissue is removed and there is no vaginal advancement. Most published results are based on vestibulectomy with vaginal advancement. It is difficult to compare the results of surgery studies because different outcome measures are used and the length of follow-up time differs. Overall success rates for both procedures range from 60-96 percent. After surgery, physical and dilator therapy are often recommended and may help alleviate any remaining pelvic floor muscle abnormalities. Careful patient selection is essential because it increases the likelihood of success with a surgical procedure. Researchers are studying factors that may predict surgical treatment success or failure; however, no conclusions can be drawn at this time.
The treatments described above are, by far, the most common ones, but your provider may recommend another approach for your specific case. These might include:
- Topical Steroids: Topical steroids are used to reduce inflammation in the vulvar tissue. If your provider thinks that inflammation is a factor, he/she may recommend steroids, which are generally used for short periods of time.
- Interferon Injections: Interferon is a substance produced by the body that helps to fight infection. In some cases, a series of injections of manufactured interferon have been injected into the vulva. Although initial studies of interferon appeared promising, recent studies indicate that interferon is not effective.
- Topical Cromolyn: Cromolyn, commonly used to treat asthma due to allergy, is a synthetic compound that prevents mast cells, which are immune system mediators of inflammatory reactions, from releasing certain chemicals. In recent years, some researchers have implicated mast cells in the etiology of vulvar vestibulitis syndrome. Cromolyn can be compounded into a topical preparation and applied directly to the vulva. An initial study showed little efficacy, but patients in this study had suffered from vulvodynia for a long time and had tried many other treatments that didn’t work. At this time, there is no information on the efficacy of cromolyn in newly diagnosed patients.
- Subcutaneous Steroid/Anesthetic Injections: In a few publications, women have reported symptom improvement after undergoing a series of steroid/anesthetic injections into the vestibule or other vulvar tissue. These injections are usually administered one week apart for several weeks.
- Botox Injections: Botox, a toxic protein produced by a certain bacteria, is sometimes used to treat muscle spasm. Recent studies have indicated that it may also interfere with pain transmission. For women with vulvodynia and pelvic floor muscle spasm, Botox is injected directly into the area(s) of spasm.
- Topical Capsaicin: Capsaicin, a component of chili peppers causing skin irritation, is currently used in topical ointments to relieve neuropathic and other types of pain. With repeated application of capsaicin, neurotransmitter levels in nerve cells diminish, leading to a reduction in pain transmission. Initial reports of capsaicin use in women with vulvodynia indicated moderate pain relief and less pain during intercourse.
- Low-Oxalate Diet and Calcium Citrate Supplementation: The recommendation that women follow a low-oxalate diet and take calcium citrate is questionable. A small percentage of women have reported some relief with this regimen. Controlled studies, however, have shown no difference in the amount of urinary oxalates excreted by women with vulvodynia and healthy controls. Some practitioners have noted that the low oxalate diet is detrimental to one’s overall health.
Managing Breakthrough Pain
Sometimes a relatively brief ‘pain flare’ escalates suddenly and ‘breaks through’ your regular pain management regimen. In addition to your long-term treatment strategy, it is important to discuss with your provider how to handle a pain flare. In many cases, he/she will write a prescription for a short-acting narcotic, such as hydrocodone.
Looking Ahead
It is important to keep in mind that research on vulvodynia is ongoing, with current studies investigating both its causes and the efficacy of different treatments. To view a summary of research studies that are in need of participants, please visit NVA’s web site.